
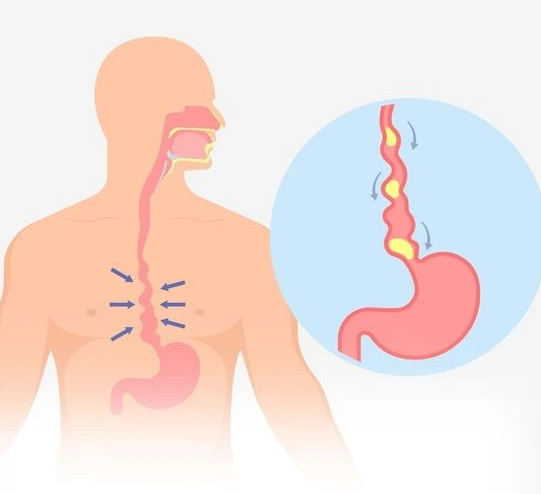
GERD/Acid reflux
GERD (gastroesophageal reflux disease) or acid reflux is a condition in which stomach acid flows back into the esophagus, the tube that connects your mouth and stomach. This happens when the lower esophageal sphincter, a ring of muscle that acts like a valve between the esophagus and stomach, doesn't close properly or relaxes too frequently.
Symptoms
The symptoms of GERD (gastroesophageal reflux disease) or acid reflux can vary from person to person, but the most common symptoms include:
- Heartburn: a burning sensation in the chest that often occurs after eating or when lying down.
- Regurgitation: the feeling of stomach contents coming back up into the throat or mouth, often accompanied by a sour taste.
- Difficulty swallowing: feeling like food or liquids are stuck in the throat or chest.
- Chest pain: discomfort or pain in the chest, especially after eating, which can be mistaken for a heart attack.
- Chronic cough: a persistent cough that is often worse at night.
- Hoarseness or sore throat: a scratchy or irritated throat, which can be caused by the acid from the stomach irritating the vocal cords.
- Asthma-like symptoms: wheezing, shortness of breath, or a feeling of tightness in the chest, which can be triggered by acid reflux.
It's important to note that not everyone with GERD experiences all of these symptoms, and some people may not experience any symptoms at all.
Causes
Several factors can contribute to the development of GERD, including:
- Hiatal hernia is a part of the stomach that pushes up into the chest through the diaphragm, which can cause the LES to malfunction.
- Obesity or being overweight can put pressure on the abdomen, which can cause the LES to open and allow acid to reflux.
- Pregnancy: Hormonal changes and the pressure of the growing fetus on the abdomen can cause the LES to relax, leading to acid reflux.
- Spicy, acidic, or fatty foods, as well as caffeine, alcohol, and carbonated beverages, can trigger or worsen GERD symptoms.
- Smoking: Nicotine can weaken the LES, making it easier for stomach acid to reflux into the esophagus.
- Medications: Certain medications, such as aspirin, ibuprofen, and some blood pressure medications, can increase the risk of GERD.
- Genetic factors: Some people may have a genetic predisposition to GERD.

Diagnosis & Treatment
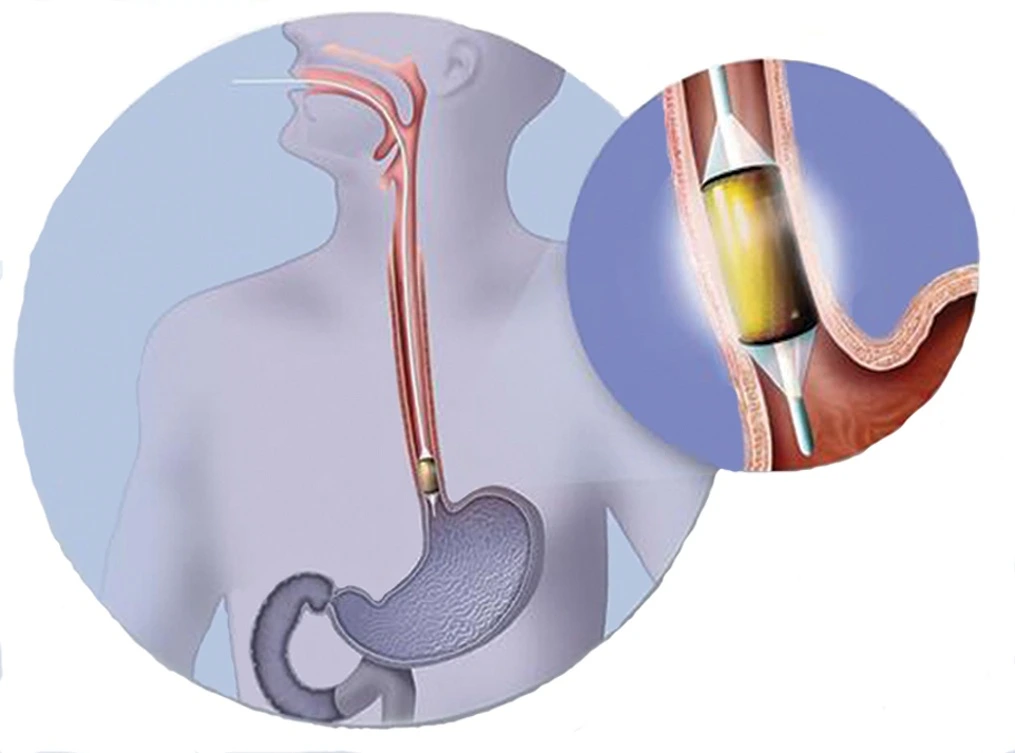
The diagnosis of GERD (gastroesophageal reflux disease) typically involves a combination of a patient's medical history, physical examination, and diagnostic tests.. Diagnostic tests that can help diagnose GERD include:
- Esophageal pH monitoring: This involves placing a small tube through the nose or mouth into the esophagus to measure the amount of acid present over a 24-hour period.
- Endoscopy: This involves passing a small camera through the mouth and into the esophagus to look for signs of inflammation or damage.
- Upper GI series: This involves drinking a contrast material and taking x-rays to look for signs of GERD.
Treatment for GERD often involves a combination of lifestyle modifications, medications, and in some cases, surgery. Lifestyle modifications may include:
- Avoiding trigger foods and drinks such as spicy, acidic, or fatty foods, caffeine, alcohol, and carbonated beverages.
- Losing weight if you are overweight or obese.
- Elevating the head of your bed.
- Eating smaller, more frequent meals.
- Quitting smoking.
Medications that may be used to treat GERD include:
- Proton pump inhibitors (PPIs): These medications reduce the production of stomach acid, which can help alleviate GERD symptoms and promote healing of the esophagus.
- H2 receptor blockers: These medications reduce the production of stomach acid, but not as strongly as PPIs.
- Antacids: These medications neutralize stomach acid and can provide short-term relief of GERD symptoms.
- Surgery: This may involve reinforcing the LES or creating a new valve to prevent stomach acid from flowing back into the esophagus.
- Newer endoscopic treatments :ARMA-Antireflux mucosal ablation, Stretta and GERDx
What to expect after treatment
With proper treatment and management, most people with GERD can expect to experience relief from their symptoms and an improvement in their overall quality of life.
Lifestyle modifications such as avoiding trigger foods and drinks, losing weight, and elevating the head of the bed can help reduce GERD symptoms and improve overall health.
Medications such as proton pump inhibitors (PPIs) or H2 receptor blockers can also help reduce acid reflux symptoms and promote healing of the esophagus. These medications may be taken for a specific period of time or may need to be continued long-term, depending on the severity of the GERD.
After surgery, patients may need to follow a specific diet or make other lifestyle modifications to promote healing and prevent complications.
Barrett's esophagus
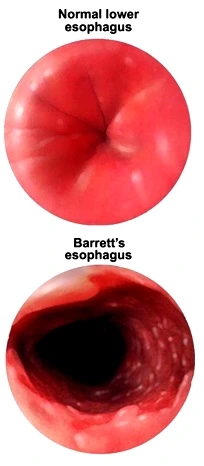
Barrett's esophagus is a medical condition in which the tissue lining the lower part of the esophagus, the tube that connects the mouth to the stomach, is replaced by tissue that is similar to that found in the lining of the intestine. This change in tissue is caused by long-term exposure to acid reflux, which can irritate and damage the normal lining of the esophagus.
Symptoms
Barrett's esophagus itself may not cause any noticeable symptoms, but it is often associated with gastroesophageal reflux disease (GERD), which can cause symptoms such as:
- Frequent heartburn or acid reflux
- Difficulty swallowing (dysphagia)
- Chest pain or discomfort
- Regurgitation of food or acid
- Nausea or vomiting
- Hoarseness or chronic cough
- Unintentional weight loss
Causes
GERD occurs when the muscle that separates the esophagus from the stomach (the lower esophageal sphincter) relaxes and allows stomach acid and other digestive fluids to flow back into the esophagus. Over time, this acid exposure can cause changes in the lining of the esophagus, leading to the development of Barrett's esophagus.
Diagnosis & Treatment
Diagnosis of Barrett's esophagus usually involves an endoscopy, which is a procedure in which a flexible tube with a light and camera is inserted into the esophagus to examine the lining. During the endoscopy, a biopsy (a small tissue sample) of the lining of the esophagus is taken to determine whether there are any abnormal changes.
If you are diagnosed with Barrett's esophagus, you will likely be recommended regular follow-up endoscopies to monitor the progression of the condition and check for any signs of cancer.
Treatment options for Barrett's esophagus may include:
- Medications to reduce acid reflux: Proton pump inhibitors (PPIs) are commonly used to reduce the amount of acid produced by the stomach and prevent reflux.
- Lifestyle changes: Avoiding foods that trigger reflux, losing weight, and avoiding smoking and alcohol can help reduce the severity of symptoms.
- Endoscopic treatment: Endoscopic therapies, such as radiofrequency ablation or cryotherapy, can be used to destroy the abnormal tissue in the esophagus.
- Surgery: In some cases, surgery may be recommended to remove the affected tissue in the esophagus.
What to expect after treatment
In general, people with Barrett's esophagus who receive appropriate treatment and follow-up care have a good prognosis. After treatment, you can expect to undergo regular follow-up endoscopies to monitor the progress of the condition and check for any signs of cancer. Your healthcare provider may also recommend lifestyle changes, such as avoiding trigger foods, losing weight, and quitting smoking, to help prevent reflux and reduce the risk of complications.
If you undergo endoscopic treatment or surgery, you may experience some temporary side effects, such as sore throat, difficulty swallowing, and abdominal pain. These side effects typically resolve within a few days to a week after the procedure.
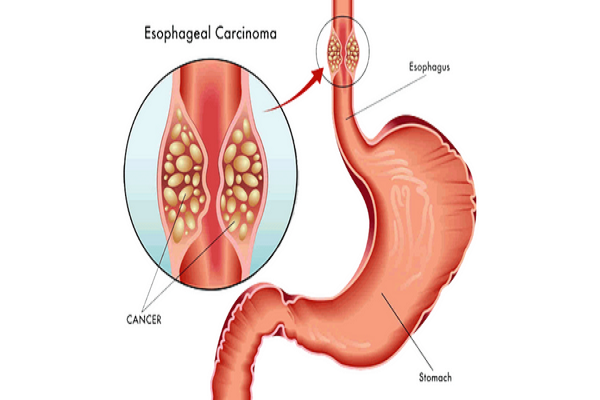
Esophageal Cancer
Esophageal cancer is a type of cancer that develops in the cells lining the esophagus, which is the muscular tube that connects the throat to the stomach. Esophageal cancer typically starts in the inner layer of cells and can grow and spread to other parts of the body.
There are two main types of esophageal cancer:
1.Squamous cell carcinoma: This type of cancer develops in the thin, flat cells that line the upper part of the esophagus.
2.Adenocarcinoma: This type of cancer develops in the glandular cells that are found in the lower part of the esophagus.
Symptoms
The symptoms of esophageal cancer can vary depending on the stage and location of the cancer. Some common symptoms include:
- Difficulty swallowing (dysphagia)
- Chest pain or discomfort
- Unintended weight loss
- Hoarseness in throat
- Persistent Coughing
- Indigestion or heartburn
- Vomiting
Causes
There are several factors known to increase the risk of developing this type of cancer.
- Esophageal cancer is more common in people over the age of 50.
- Men are more likely than women to develop esophageal cancer.
- Smoking or using other tobacco products increases the risk of esophageal cancer.
- Drinking alcohol in excess can damage the lining of the esophagus and increase the risk of cancer.
- Gastroesophageal reflux disease (GERD)
- Barrett's esophagus
- Being overweight or obese increases the risk of esophageal cancer.
- Having a family history of esophageal cancer
Diagnosis & Treatment
Diagnosis of esophageal cancer usually involves several tests, including:
- Endoscopy.
- Biopsy
- Imaging tests such as CT scans, PET scans etc
- Blood tests
The main treatment options for esophageal cancer include:
- Surgery: Surgery may be used to remove the cancerous tissue and nearby lymph nodes. Depending on the location and extent of the cancer, different types of surgery may be used, including esophagectomy (removal of part or all of the esophagus), gastrectomy (removal of part or all of the stomach), or a combination of the two.
- Radiation therapy: Radiation therapy uses high-energy X-rays or other types of radiation to kill cancer cells.
- Chemotherapy: Chemotherapy uses drugs to kill cancer cells throughout the body.
- Targeted therapy: Targeted therapy uses drugs that specifically target certain proteins or other molecules that are involved in the growth and spread of cancer cells.
- Immunotherapy: Immunotherapy uses drugs to stimulate the body's immune system to attack cancer cells.
- Palliative care: Palliative care focuses on relieving symptoms and improving quality of life for patients with advanced or metastatic esophageal cancer.
What to expect after treatment
Generally, patients can expect to experience some pain, discomfort, and fatigue for several weeks following the procedure.
Here are some common things that you can expect after esophageal cancer surgery:
1.Hospital Stay: After the surgery, you will stay in the hospital for a few days, typically 5-10 days, depending on the extent of the surgery and how quickly you recover.
2.Pain Management: You will likely experience pain or discomfort at the incision site or the chest area. Pain management is an important part of recovery, and you will receive pain medication as needed.
3.Diet Changes: After surgery, your doctor may advise you to stick to a soft or liquid diet for a while. It may take some time for you to adjust to eating normally again.
4.Physical Therapy: Depending on the extent of the surgery and how long you were in the hospital, you may need physical therapy to help you regain your strength and mobility.
5.Follow-Up Care: After the surgery, you will have regular follow-up appointments with your doctor to monitor your recovery and check for any signs of cancer recurrence.

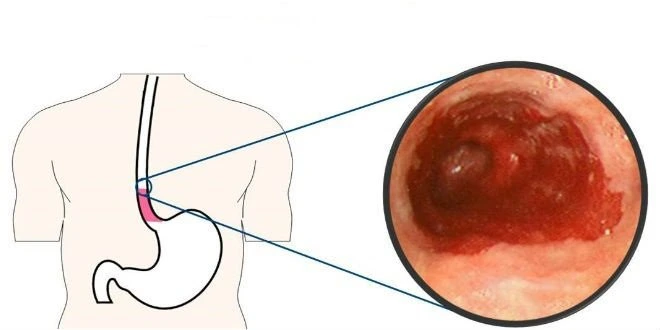
Esophageal Ulcer
An esophageal ulcer is a sore or lesion that develops in the lining of the esophagus, which is the tube that connects the throat to the stomach. Esophageal ulcers can be painful and can cause difficulty in swallowing, and they are typically caused by long-term acid reflux.
There are two main types of esophageal ulcers:
1.Peptic Ulcer: This type of ulcer is caused by stomach acid that flows back into the esophagus. Peptic ulcers are often associated with gastroesophageal reflux disease (GERD) and can cause pain or burning in the chest area.
2.Infectious Ulcer: This type of ulcer is caused by an infection, usually with a bacteria called Helicobacter pylori. Infectious ulcers are less common than peptic ulcers.
Symptoms
Some common symptoms of esophageal ulcer include:
- Pain or discomfort in the chest or upper abdomen.
- Difficulty in swallowing
- Nausea or vomiting
- Indigestion or heartburn
- Weight loss: If the ulcer is severe or long-lasting, it can cause weight loss due to difficulty in eating or absorption of nutrients.
- Blood in vomit or stool: In some cases, an esophageal ulcer can lead to bleeding, which can result in the presence of blood in vomit or stool.
Causes
The most common cause of esophageal ulcers is gastroesophageal reflux disease (GERD). However, other factors may contribute to the development of an esophageal ulcer, including:
- Helicobacter pylori, a type of bacteria that can cause stomach ulcers, has also been linked to esophageal ulcers.
- Certain medications can increase the risk of developing esophageal ulcers.
- Smoking
- Heavy alcohol consumption
- Radiation therapy to the chest or neck
- Swallowing of corrosive substances
- Genetic factors
Diagnosis & Treatment
Diagnosis of an esophageal ulcer typically involves a combination of medical history, physical examination, and diagnostic tests. an endoscopy to examine the inside of the esophagus and stomach and look for signs of ulceration may be performed. During the endoscopy, a biopsy may also be taken to check for signs of infection or other underlying conditions.
The main goals of treatment are to reduce pain, promote healing of the ulcer, and prevent complications.
- Medications: Depending on the cause of the ulcer, medications may be prescribed to treat the underlying condition and reduce stomach acid production.
- Antibiotics: If the ulcer is caused by a bacterial infection, antibiotics may be prescribed to eliminate the bacteria.
- Surgery: In rare cases, surgery may be necessary to treat an esophageal ulcer that is not responding to other treatments or has caused serious complications like perforation.
- Lifestyle changes: Making changes to your lifestyle can help reduce the risk of developing an esophageal ulcer and prevent symptoms from worsening.
- Avoidance of irritants: Avoiding certain medications like NSAIDs, aspirin, and bisphosphonates that can increase the risk of developing esophageal ulcers.
- Nutritional support: In some cases, nutritional support may be necessary to help promote healing of the ulcer and prevent weight loss.
What to expect after treatment
After treatment for an esophageal ulcer, the symptoms should start to improve within a few days to a few weeks
1.Relief of symptoms: As the ulcer heals, you should notice a reduction in symptoms like chest pain, difficulty swallowing, and heartburn.
2.Follow-up appointments: Your doctor may recommend regular follow-up appointments to monitor the healing of the ulcer and adjust treatment as necessary.
3.Lifestyle modifications: To prevent the recurrence of the ulcer or the development of new ulcers, your doctor may recommend making lifestyle modifications like quitting smoking, avoiding certain foods, and reducing alcohol consumption.
4.Medications: Depending on the cause of the ulcer, your doctor may prescribe medications like PPIs or H2 blockers to reduce acid production and promote healing.
5.Nutritional support: If you have experienced significant weight loss due to the ulcer, your doctor may recommend nutritional support to help you regain lost weight and prevent malnutrition.
6.Prevention of complications: In some cases, an esophageal ulcer can lead to serious complications like bleeding, perforation, or strictures (narrowing of the esophagus). Your doctor will monitor you closely to prevent these complications from occurring.

Esophageal Varices
Esophageal varices are enlarged and swollen veins in the lining of the lower esophagus, which can occur due to increased pressure in the veins that bring blood from the digestive tract to the liver
Symptoms
Esophageal varices may not cause any symptoms until they rupture and bleed. However, some people with esophageal varices may experience symptoms such as:
- Pain or discomfort in the upper abdomen
- Black, tarry, or bloody stools
- Vomiting blood or material that looks like coffee grounds
- Dizziness or lightheadedness
- Rapid or irregular heartbeat
- Low blood pressure
Causes
In some conditions, such as liver cirrhosis, portal vein thrombosis, or other liver diseases, the liver is unable to process blood efficiently, causing pressure to build up in the portal vein. This increased pressure can cause the veins in the esophagus to become swollen and engorged, forming varices.
Other factors that may increase the risk of developing esophageal varices include alcohol abuse, viral hepatitis (such as hepatitis B or C), and certain genetic disorders that affect the liver. Additionally, certain medications and blood thinners can also increase the risk of developing esophageal varices by irritating the lining of the esophagus and causing bleeding. In some rare cases, esophageal varices can be caused by conditions such as portal vein thrombosis or splenic vein thrombosis.

Diagnosis & Treatment
Diagnosis of esophageal varices typically involves an endoscopy, During the endoscopy, the doctor can visualize the varices and assess their size and severity. If varices are found, the doctor may also perform a biopsy to check for signs of liver disease.
Treatment of esophageal varices aims to reduce the risk of bleeding and prevent complications. Some treatment options include:
- Medications: Drugs called beta-blockers can be used to reduce the pressure in the veins and prevent bleeding. Other medications may be used to treat underlying conditions that contribute to the development of varices, such as antiviral medications for hepatitis B or C.
- Endoscopic therapy: Endoscopic treatments, such as band ligation or sclerotherapy, can be used to seal off the varices and reduce the risk of bleeding.
- Transjugular intrahepatic portosystemic shunt (TIPS): TIPS is a procedure that involves creating a shunt (or bypass) between the portal vein and the hepatic vein to reduce pressure in the veins and prevent bleeding.
- Surgery: In some cases, surgery may be necessary to remove the varices or perform a liver transplant if the liver is severely damaged.
What to expect after treatment
The specific expectations and outcomes will depend on the type of treatment received and the severity of the varices. If medications were prescribed, you may need to take them long-term to reduce the risk of bleeding and prevent the varices from returning If endoscopic therapy or TIPS was performed, you may experience some discomfort or difficulty swallowing for a short period after the procedure. a soft or liquid diet will be recommended for a few days after the procedure to allow your esophagus to heal. You may also be prescribed medications to relieve pain or reduce inflammation.
In some cases, a repeat endoscopy may be needed to monitor the varices and assess the effectiveness of the treatment. It is important to follow a healthy diet and lifestyle to prevent further damage to the liver and reduce the risk of complications. Avoiding alcohol and maintaining a healthy weight can also be beneficial.
