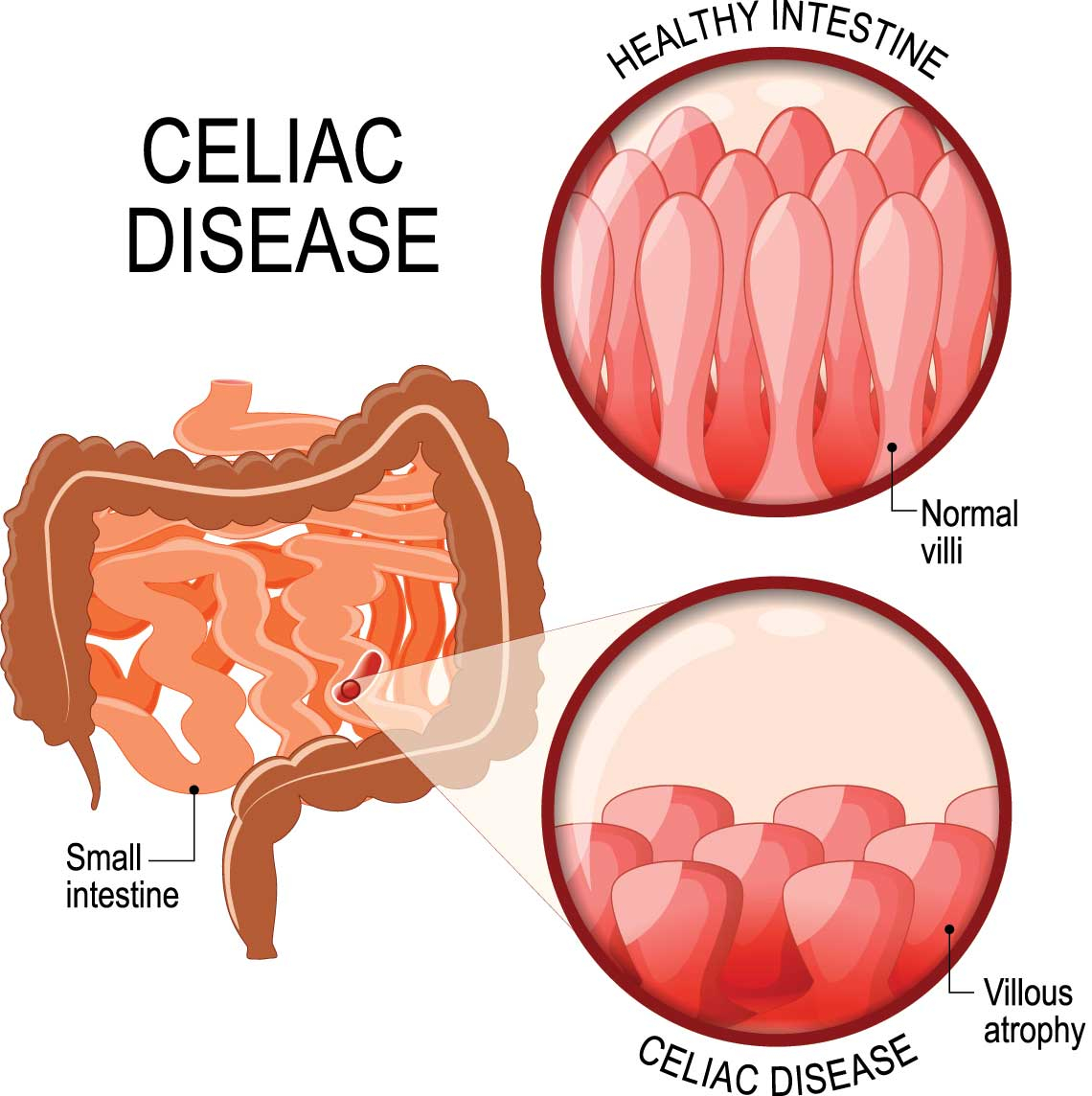
Celiac Disease
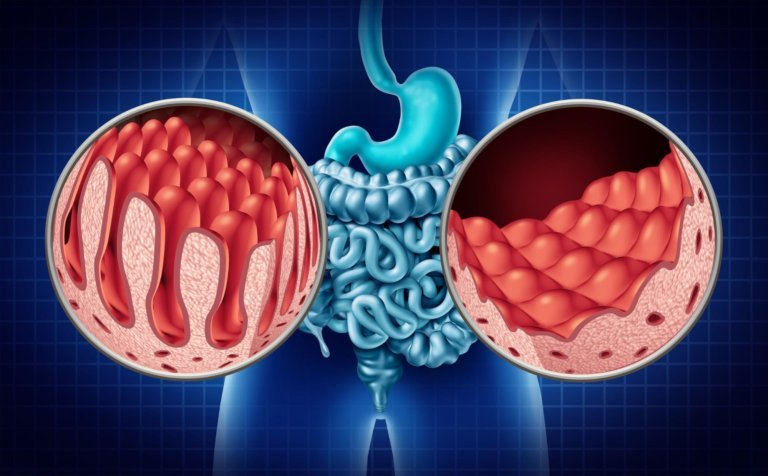
Celiac disease, also known as coeliac disease, is a chronic autoimmune disorder of the small intestine that occurs in genetically predisposed individuals. When people with celiac disease eat foods containing gluten, their immune system responds by damaging the lining of the small intestine.
Symptoms
The most common symptoms of celiac disease are related to the digestive system and can include:
- Abdominal pain and bloating
- Diarrhea or constipation
- Nausea and vomiting
- Gas and flatulence
- Weight loss or difficulty gaining weight
However, celiac disease can also cause a range of non-gastrointestinal symptoms, including:
- Anemia (low iron levels in the blood)
- Fatigue and weakness
- Bone and joint pain
- Headaches and migraines
- Skin rash or dermatitis herpetiformis (a chronic skin condition)
Causes
Celiac disease is caused by a combination of genetic and environmental factors. In people with celiac disease, the immune system reacts to gluten, a protein found in wheat, barley, and rye, as if it were a foreign invader.
It is believed to be triggered by a combination of genetic susceptibility and environmental factors such as infections, surgery, or emotional stress. People with a family history of celiac disease are more likely to develop the condition, as are those with other autoimmune disorders such as type 1 diabetes or rheumatoid arthritis.
Diagnosis & Treatment
The diagnosis of celiac disease typically involves a combination of blood tests, genetic testing, and a biopsy of the small intestine. A blood test can detect antibodies that the body produces in response to gluten, while genetic testing can identify whether a person carries certain genes that increase the risk of celiac disease.
The only effective treatment for celiac disease is a lifelong gluten-free diet. This means avoiding all foods that contain wheat, barley, rye, and related grains, as well as foods that may have come into contact with gluten during processing. In some cases, people with celiac disease may also need to take supplements to address any nutritional deficiencies caused by malabsorption in the small intestine.
In rare cases, some people with celiac disease may not respond to a gluten-free diet and may require additional treatment or medication.
What to expect after treatment
After treating celiac disease with a strict gluten-free diet, most people can expect to experience significant improvement in their symptoms and quality of life.The amount of time it takes for the small intestine to heal can vary depending on the severity of the damage and how long a person has had celiac disease before diagnosis.Over time, as the small intestine heals, people with celiac disease can expect to see improvements in their nutrient absorption and overall health.
Patients need to be careful about reading food labels, avoiding cross-contamination, and being aware of hidden sources of gluten in medications, supplements, and other products.
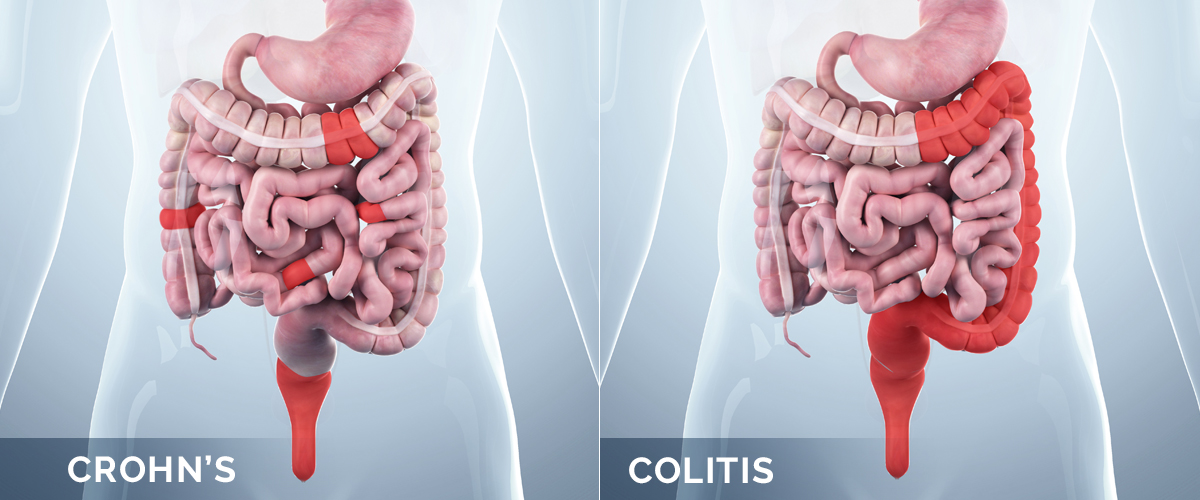
Crohns Disease
Crohn's disease is a chronic inflammatory bowel disease that primarily affects the digestive tract. It can affect any part of the digestive system, from the mouth to the anus, but most commonly affects the small intestine and the beginning of the large intestine.
Symptoms
The symptoms of Crohn's disease can vary depending on the severity and location of inflammation in the digestive tract. Some common symptoms of Crohn's disease may include:
- Abdominal pain and cramping
- Diarrhea
- Rectal bleeding
- Fatigue
- Weight loss
- Loss of appetite
- Anemia
- Fever
- Mouth sores
- Joint pain and inflammation
- Skin rashes
- Eye inflammation
Causes
Here are some of the factors that may contribute to the development of Crohn's disease:
- Genetics: people with a family history of Crohn's disease are more likely to develop the condition, suggesting a genetic component.
- Immune system dysfunction: It is believed that an abnormal immune response may trigger inflammation in the digestive tract, leading to Crohn's disease.
- Environmental factors: Certain environmental factors, such as a diet high in sugar and processed foods, smoking, and stress, may trigger or exacerbate symptoms of Crohn's disease.
- Gut microbiome: An imbalance in the gut microbiome, the community of bacteria and other microorganisms that inhabit the digestive tract, may contribute to the development of Crohn's disease.
- Other factors: Previous gastrointestinal infections, use of certain medications, and a history of autoimmune disorders may also increase the risk of developing Crohn's disease.

Diagnosis & Treatment
Diagnosis of Crohn's disease typically involves a combination of medical history review, physical examination, imaging tests, and laboratory tests such as blood tests, stool tests, colonoscopy, endoscopy, CT scans, or MRI scans to evaluate the condition of the digestive tract.
Treatment of Crohn's disease is typically aimed at reducing inflammation, relieving symptoms, and preventing complications.
- Medications such as anti-inflammatory drugs, corticosteroids, immunosuppressants, and biologic therapies may be used to reduce inflammation and manage symptoms.
- A healthy diet, avoiding trigger foods and ensuring adequate nutrition can help reduce symptoms and improve overall health.
- Quitting smoking, reducing stress, and regular exercise can help manage symptoms.
- Surgery may be necessary in severe cases of Crohn's disease to remove damaged portions of the digestive tract or to correct complications such as bowel obstruction.
What to expect after treatment
With appropriate medical care, most people with Crohn's disease can achieve remission.
Here's what you can expect after treatment of Crohn's disease:
1.With successful treatment, you can expect to experience improved quality of life, including less pain, less frequent bowel movements, and less disruption to your daily activities.
2.Treatment can help manage symptoms such as diarrhea, abdominal pain, and rectal bleeding.
3.Treatment can also help reduce complications such as intestinal blockages, abscesses, and fissures.
4.It's important to continue to work closely with your healthcare provider to monitor your condition regularly and adjust treatment as necessary to maintain remission.
5.While treatment can be effective in controlling Crohn's disease, it is possible for flare-ups to occur, so it's important to be aware of the signs and symptoms and seek prompt medical attention if they occur.
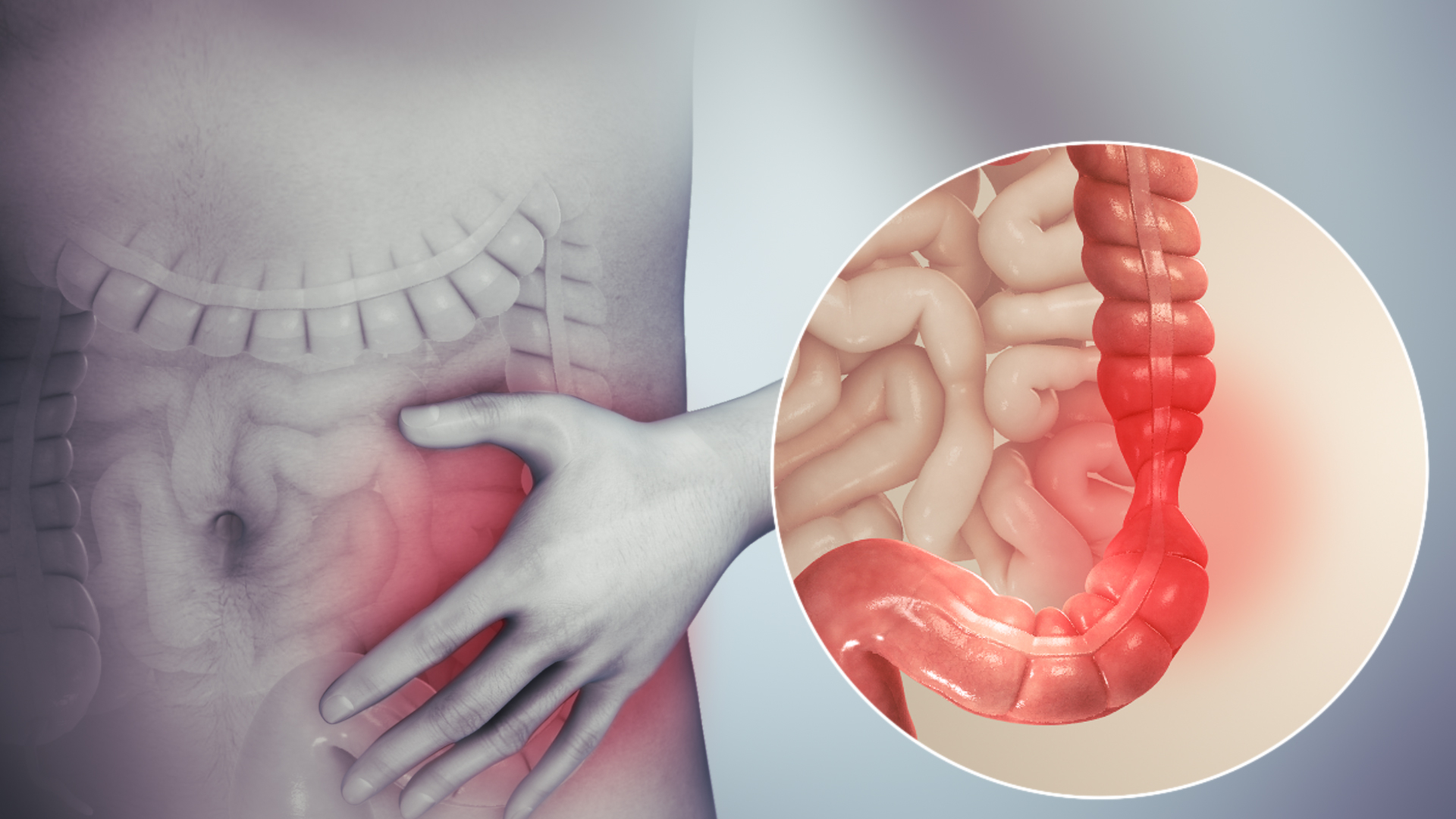
IBS
IBS stands for Irritable Bowel Syndrome, which is a common gastrointestinal disorder that affects the large intestine or colon. It is a chronic condition characterized by a group of symptoms that can include abdominal pain, bloating, gas, diarrhea, and/or constipation.
Symptoms
However, the most common symptoms of IBS include:
- Abdominal Pain or Discomfort
- Bloating
- Gas
- Diarrhea
- Constipation
- Alternating Diarrhea and Constipation
- Mucus in Stool
- Nausea
Causes
IBS is caused by a combination of factors that can include:
- Abnormal Gastrointestinal Motility: IBS is associated with changes in the way the muscles of the intestines contract and move food through the digestive system.
- Abnormal Nervous System Signaling: The nerves in the gastrointestinal tract can be hypersensitive in people with IBS, leading to pain and discomfort even with normal contractions of the intestines.
- Food Sensitivities: Some people with IBS may have sensitivities to certain foods or food additives, which can trigger symptoms.
- Abnormal Gut Microbiome: An imbalance of microorganisms (The collection of microorganisms) may contribute to IBS symptoms.
- Psychological Factors: Stress, anxiety, and depression can all contribute to IBS symptoms, although they do not directly cause the condition.
- Genetics: There may be a genetic component to IBS, as it is more common in people who have a family history of the condition.

Diagnosis & Treatment
Diagnosis of IBS typically involves a combination of medical history review, physical examination, imaging tests, and laboratory tests such as blood tests, stool tests, colonoscopy, endoscopy, CT scans, or MRI scans to evaluate.
There is no cure for IBS, but treatment focuses on managing symptoms and improving quality of life.
Treatment may include:
- Dietary Changes
- Medications
- Stress Reduction
- Exercise
- Probiotics
What to expect after treatment
After treatment for Irritable Bowel Syndrome (IBS), many people experience significant relief from their symptoms and an improvement in their overall quality of life. it's important to continue to manage symptoms and follow a healthy lifestyle to prevent future flare-ups.Overall, the goal of IBS treatment is to manage symptoms and improve quality of life. Lifestyle changes, such as following a healthy diet, getting regular exercise, and managing stress levels, can also help reduce the severity and frequency of IBS symptoms.

Whipple’s disease
Whipple's disease is a rare bacterial infection that primarily affects the digestive system. The condition is caused by a type of bacteria called Tropheryma whipplei, which can infect various organs in the body, including the intestines, joints, and brain.
Symptoms
Common symptoms of Whipple's disease include:
- Diarrhea, abdominal pain, and bloating are common symptoms of Whipple's disease. Malabsorption of nutrients may also occur, leading to weight loss and malnutrition.
- Joint pain and stiffness are common symptoms of Whipple's disease, and may affect multiple joints in the body.
- In some cases, Whipple's disease can cause neurological symptoms, including memory loss, confusion, and seizures.
- Chronic fatigue is a common symptom of Whipple's disease, and may be severe enough to interfere with daily activities.
- Some people with Whipple's disease may develop eye symptoms, such as uveitis or other inflammation of the eye.
- A low-grade fever may occur in some people with Whipple's disease.
Causes
Whipple's disease is caused by a type of bacteria called Tropheryma whipplei. It is believed that the bacteria may be present in the environment and can enter the body through the digestive system.
Certain factors may increase the risk of developing Whipple's disease, including a weakened immune system, genetic predisposition, and exposure to certain environmental triggers.

Diagnosis & Treatment
Diagnosing Whipple's disease can be challenging because its symptoms can mimic those of other conditions. A definitive diagnosis is made by identifying the bacterium in a tissue sample, typically from the small intestine. Blood tests, stool tests, and imaging studies such as CT scans and MRI may also be used to help diagnose the disease.
Whipple's disease requires long-term antibiotic therapy to completely eliminate the bacteria from the body. The initial treatment usually consists of a combination of antibiotics followed by an oral antibiotic regimen for up to a year.
In some cases, symptoms may persist despite antibiotic therapy. Additional treatments may be necessary to manage these symptoms, such as corticosteroids for joint inflammation or medications to control diarrhea.
What to expect after treatment
After successful treatment of Whipple's disease, most patients experience significant improvement in their symptoms. In the immediate aftermath of treatment, patients may still experience some symptoms of the disease, such as fatigue, joint pain, or gastrointestinal disturbances. These symptoms usually improve gradually over several weeks or monthsLong-term follow-up care is crucial to monitor for any signs of disease recurrence with appropriate treatment and careful monitoring, most patients with Whipple's disease can expect to make a full recovery and return to their normal daily activities
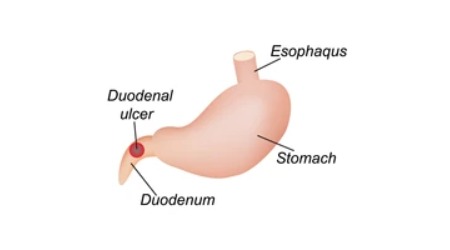
Duodenal ulcer
A duodenal ulcer is a type of peptic ulcer that develops in the lining of the first part of the small intestine, called the duodenum. Peptic ulcers are open sores that form in the lining of the stomach, esophagus, or duodenum, and are usually caused by the presence of stomach acid and digestive juices that erode the protective lining of these organs.
Symptoms
However, common symptoms of a duodenal ulcer may include:
- Burning or gnawing pain in the upper abdomen that may improve or worsen with eating
- Nausea and vomiting
- Feeling of fullness or bloating in the upper abdomen
- Heartburn or acid reflux
- Unintentional weight loss
- Loss of appetite
- Dark, tarry stools (a sign of bleeding in the digestive tract)
In some cases, a duodenal ulcer can cause complications such as bleeding, perforation (a hole in the wall of the duodenum), or obstruction. These complications can cause more severe symptoms such as sudden, severe abdominal pain, bloody or black stools, difficulty breathing, and feeling faint or dizzy.
Causes
Duodenal ulcers are usually caused by a combination of factors, including:
- Helicobacter pylori (H. pylori) infection: This bacterium is a common cause of duodenal ulcers. It can damage the protective lining of the stomach and duodenum, making them more vulnerable to the effects of stomach acid and digestive juices.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): Long-term use of NSAIDs, such as aspirin, ibuprofen, and naproxen, can irritate the lining of the stomach and duodenum, leading to the development of ulcers.
- Excess acid production: Certain conditions, such as Zollinger-Ellison syndrome, can cause the stomach to produce too much acid, which can lead to the development of ulcers.
- Smoking: Smoking can increase the risk of developing duodenal ulcers and can also delay healing of existing ulcers.
- Stress: While stress alone does not cause ulcers, it can exacerbate symptoms and delay healing.
- Genetics: Some people may be more susceptible to duodenal ulcers due to genetic factors.

Diagnosis & Treatment
Diagnosis of a duodenal ulcer usually involves a combination of medical history, physical examination, and diagnostic tests
- Endoscopy: A procedure that uses a thin, flexible tube with a camera to examine the inside of the esophagus, stomach, and duodenum.
- Upper gastrointestinal (GI) series: A test that uses X-rays and a contrast material to examine the upper digestive tract.
- Blood, stool, or breath tests: These tests can detect the presence of H. pylori bacteria in the body.
Treatment options may include:
- Antibiotics: If an H. pylori infection is present, a course of antibiotics may be prescribed to eradicate the bacteria.
- Acid-reducing medications: Proton pump inhibitors (PPIs) and histamine H2-receptor blockers can reduce the amount of acid produced by the stomach and help promote healing of the ulcer.
- Antacids: These medications can help neutralize stomach acid and provide temporary relief of symptoms.
- Lifestyle changes: Quitting smoking, avoiding alcohol, eating a healthy diet, and managing stress can all help improve symptoms and prevent future ulcers.
In rare cases, surgery may be necessary to treat a duodenal ulcer that does not respond to other treatments or that causes complications such as bleeding or perforation.
What to expect after treatment
After successful treatment of a duodenal ulcer, you can expect to experience relief from symptoms such as pain and discomfort in the upper abdomen. Follow-up testing will be required to ensure that the infection has been eradicated. You may also need to continue taking acid-reducing medications for several weeks to allow the ulcer to heal completely.
It is important to continue following a healthy lifestyle to prevent future ulcers. This may include avoiding alcohol and smoking, eating a balanced diet, and managing stress

Abdominal/Small intestine TB
Abdominal or small intestine tuberculosis (TB) is a type of extrapulmonary TB that affects the gastrointestinal tract, particularly the small intestine. It is caused by the bacterium Mycobacterium tuberculosis, which can infect various parts of the body.
Symptoms
Symptoms of abdominal/small intestine TB can vary, but may include:
- Abdominal pain
- Diarrhea
- Loss of appetite
- Weight loss
- Fatigue
- Fever
- Nausea and vomiting
Causes
Abdominal tuberculosis (TB) is caused by the bacterium Mycobacterium tuberculosis, which can affect various organs in the body, including the lungs, bones, lymph nodes, and the gastrointestinal tract. When TB affects the gastrointestinal tract, it can cause inflammation and damage to the lining of the stomach or small intestine.
In the case of abdominal or small intestine TB, the bacteria can enter the body through contaminated food or water or by inhaling airborne droplets from someone with active TB disease. The bacteria can then spread to the digestive system through the bloodstream or lymphatic system.
Other factors that can increase the risk of developing abdominal TB include a weakened immune system due to conditions such as HIV, malnutrition, or diabetes, as well as certain medications that suppress the immune system.

Diagnosis & Treatment
A combination of clinical evaluation, imaging tests (such as X-rays, CT scans, or ultrasound), and laboratory tests (such as blood tests, stool tests, or biopsy) may be necessary to make a definitive diagnosis.
Treatment for abdominal or small intestine TB usually involves a combination of antibiotics that are effective against the Mycobacterium tuberculosis bacteria.
In addition to antibiotics, supportive care may be necessary to manage symptoms such as abdominal pain, diarrhea, and malnutrition. In severe cases, surgery may be required to remove damaged tissue or to repair complications such as intestinal obstruction or perforation.
What to expect after treatment
After completing the treatment for abdominal or small intestine TB, most people can expect to fully recover and return to their normal activities
Some possible outcomes after treatment for abdominal or small intestine TB may include:
1.Treatment for abdominal or small intestine TB is usually very effective, and most people experience a significant improvement in their symptoms within a few weeks of starting antibiotics.
2.After completing the full course of treatment, additional tests, such as chest X-rays or sputum cultures will be conducted to confirm that the TB infection has been fully cured.
3.In some cases, regular follow-up visits or testing to monitor for any potential complications or to ensure that the infection has not returned will be suggested
4.Antibiotics used to treat abdominal or small intestine TB can cause side effects such as nausea, vomiting, and liver damage. However, these side effects are generally rare and can be managed with close monitoring and appropriate care.
